| Original Article | ||
Open Vet. J.. 2022; 12(4): 562-566 Open Veterinary Journal, (2022), Vol. 12(4): 562–566 Original Research Comparison between the Parks Medical Doppler and the Mano Médical Vet BP Doppler for recording indirect systemic blood pressure in conscious dogsMarina Domingues1*, Panagiotis E. Archontakis1,2, Jonathan Bouvard1†, Luke Winter1 and Danielle A. Gunn-Moore11Department of Internal Medicine, The Royal (Dick) School of Veterinary Studies and The Roslin Institute, University of Edinburgh, Edinburgh, UK 2Department of Clinical Science and Services, Royal Veterinary College, University of London, London, UK †Sadly, Dr Jonathan Bouvard died in 2021; we therefore dedicate this paper to him. *Corresponding Author: Marina Domingues. The Royal (Dick) School of Veterinary Studies and The Roslin Institute, University of Edinburgh, Edinburgh, UK. Email: marina.md89 [at] gmail.com Submitted: 28/03/2022 Accepted: 14/07/2022 Published: 19/08/2022 © 2022 Open Veterinary Journal
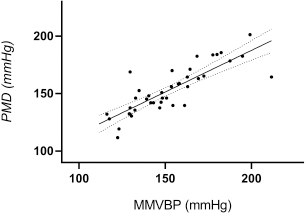
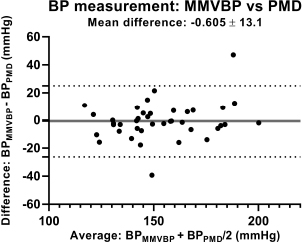
AbstractBackground: The acquisition of systemic blood pressure (SBP) provides valuable information regarding cardiovascular function and tissue perfusion in human and veterinary species. Aim: To evaluate the agreement between Parks Medical Doppler (PMD) and Mano Médical Vet BP (MMVBP) Doppler for assessing SBP in conscious dogs. Methods: 40 client-owned dogs were prospectively enrolled; SBP measurements were acquired by a single operator using the PMD and then the MMVBP. The mean of five consecutive measurements for each device was classified according to target organ damage (TOD) risk scores (1: <140 mmHg; 2: 140–160 mmHg; 3: 160–180 mmHg; 4: ≥ 180 mmHg). Results: Total mean SBP for the devices was not statistically different (p=0.77). However, the Bland–Altman analysis revealed wide limits of agreement (LoA), with MMVBP slightly underestimating SBP compared to PMD (bias=−0.6 mmHg, 95% LoA: −26.3 to 25.09). Both devices correlated well ( r=0.8269; p < 0.0001) and had identically acceptable intra-observer repeatability (coefficients of variation=4.09% for MMVBP and 3.86% for PMD). Four dogs (10%) had a TOD score of 3 by one device but scored <3 with the other. Conclusion: A good agreement and correlation was observed between the PMD and the MMVBP, suggesting that both devices can be used interchangeably for assessment of SBP in conscious dogs. The wide LoA observed between both devices was most likely associated with intraindividual variability in SBP over time. Keywords: Conscious, Dogs, Doppler, Systemic blood pressure. IntroductionThe acquisition of systemic blood pressure (SBP) provides valuable information regarding cardiovascular function and tissue perfusion in human and veterinary species. This measurement is a fundamental part of the clinical assessment for those patients in which disturbances of blood pressure are a possibility (Hsiang et al., 2008; Vachon et al., 2014). In the clinical setting, SBP assessment is vital for the diagnosis and appropriate management of patients suffering from hypertension or hypotension. Both of these disturbances can result in clinically significant and potentially irreversible tissue injury, hence the importance of its accurate detection (Littman et al., 1988; Sansom and Bodey, 1997; Finco, 2004; Haberman et al., 2006). Measurement of SBP can be accomplished by using a direct invasive method or an indirect noninvasive method (Stepien and Rapoport, 1999). The direct invasive method is considered the gold standard for blood pressure measurement in veterinary patients (Bodey et al., 1996; Wagner and Brodbelt, 1997; Stepien and Rapoport, 1999; Bosiack et al., 2010); however, it is usually obtained via intra-arterial catheterization, which requires specialized equipment and operator’s expertise. Moreover, this method can be challenging to perform in a conscious veterinary patient, where it can cause some discomfort, making it impractical to apply in clinical practice (Wagner and Brodbelt, 1997; Bosiack et al., 2010; Vachon et al., 2014). For this reason, noninvasive indirect blood pressure (NIBP) methods involving the use of an inflatable cuff and a detection device, such as Doppler ultrasonography and oscillometry, are more commonly used (Haberman et al., 2006; Vachon et al., 2014). Currently, there are numerous commercially available NIBP devices used to measure SBP in veterinary patients. However, none of these devices meet the published human validation criteria when used in conscious dogs (Acierno et al., 2018). The Parks Medical Doppler (PMD) is one of the most commonly used Doppler ultrasonography devices in veterinary practices across the world and is considered an appropriate device for NIBP measurement in conscious dogs (Haberman et al., 2006; Acierno et al., 2018). Its discontinuation from the market has prompted the need for other Doppler devices to be considered as its replacement. The Mano Médical Vet BP (MMVBP) Doppler (Mano Médical) is one of the new devices currently on the market. It benefits in its portability (compact dimensions: 0.3 kg), user-friendly interface, as well as cost-effectiveness. A consistent and comparable performance by this device might allow it to be a suitable alternative to the PMD for SBP assessment in clinical practice. We hypothesized that the MMVBP and PMD devices can be used interchangeably. To investigate this hypothesis, we evaluated the intra-observer repeatability and the level of agreement between SBP measurements obtained with the two devices when used on conscious dogs. Since there could be no comparison with direct blood pressure assessment, the study did not aim to validate these indirect devices. Materials and MethodsAnimalsClient-owned dogs referred for various medical reasons were considered for enrolment if they underwent conscious SBP measurements as part of their medical work-up. Owner consent was obtained for all participants. Dogs in which compliance was not adequate and in which the likelihood of developing handling-associated stress was high, were not included in the study, as this could contribute to significant variations in SBP, making interpretation of these readings challenging (Remillard et al., 1991). Moreover, dogs were also excluded if their participation in the study could be detrimental for their physical or mental health. Dog’s sex, age and breed were collected from the patient’s medical files. Blood pressure measurementsAll SBP measurements were obtained by a single operator in accordance with the American College of Veterinary Internal Medicine (ACVIM) consensus statement, using the same experienced handler and assistant in every case (Acierno et al., 2018). A total of six consecutive SBP measurements were carried out on all dogs with each of the two Doppler ultrasonography devices studied (811-BL; Parks Medical Electronics and Vet DP Doppler; Mano Médical); both devices were calibrated and operated according to their manufacturer’s guidelines. The PMD was the first device used in all cases. For each device, the first reading obtained was discarded (Acierno et al., 2018). The mean of five SBP values was then calculated for each device and divided according to the target organ damage (TOD) risk-scoring system (1: < 140 mmHg; 2: 140–159 mmHg; 3: 160–179 mmHg; 4: ≥ 80 mmHg) as suggested by Acierno et al. (2018). Hypotension was defined as a mean SBP < 120 mmHg (Acierno et al., 2018). Stress and anxiety were minimized by performing SBP measurements with minimal stress and gentle handing, in a quiet room, allowing a 5-minute period of acclimation to the surroundings before and between each set of measurements (Acierno et al., 2018). Dogs were gently restrained in sternal recumbency in an attempt to ensure positioning of the cuff at the level of the heart base. For practical purposes, one forelimb was chosen, and the same limb was used for all consecutive measurements. A small patch of fur, over the ulnar artery of approximately 2 cm2, was clipped below the carpal pad of the selected limb. An inflatable cuff (FlexiPort® Disposable Blood Pressure Cuffs; Welch Allyn) with a width of approximately 30%–40% of the circumference of the chosen forelimb (measured by using a soft measuring tape) was placed on the antebrachium, in accordance to the ACVIM consensus statement (Acierno et al., 2018). Care was taken to place the center of the inflatable part of the cuff on the medial aspect of the limb and the air tube on the distal end of the cuff. The concave side of the piezoelectric crystal was then covered with coupling gel and placed on the skin, distal to the cuff at the level of the previously clipped area. The pressure holding the probe in place and volume control were finely adjusted until the pulse was heard clearly through the speaker. The cuff was inflated to occlude arterial pressure until no sound was heard using a sphygmomanometer. The cuff was gradually deflated to allow return of flow through the artery until the first sound was heard at systolic pressure. Statistical analysisStatistical analysis was conducted using a commercially available statistical software (Prism 8, version 8.2.1). Data were assessed for normality graphically and tested by using the Shapiro–Wilk normality test. Continuous variables were reported as mean ± standard deviation (SD), if normally distributed, and as median and ranges, if not normally distributed. For all dogs, a single pair of measurements was used for analysis. The mean SBP from each set of five measurements obtained with both devices was calculated. Sets of pairs of values were compared with paired t-tests. Bias and limits of agreement (LoA) between both devices were assessed by a Bland–Altman plot. For the purpose of this study, “good agreement” was defined as a difference of ≤ 10 mmHg between the mean SBP obtained from both devices. Correlation (r) between the devices was determined by the Pearson correlation test and defined as excellent if r ≥ 0.90, very good if 0.90 > r ≥ 0.70, good if 0.70 > r ≥ 0.50, or poor if r < 0.50 (Hinkle et al., 2003). Coefficients of variation (CV) were defined as the SD of the differences divided by the mean of the variable under consideration and were expressed as a percentage. Values < 15% were considered adequate for clinical use (Chetboul, 2015). A two-sided alpha of p < 0.05 was considered to be statistically significant. Ethical approvalThis prospective study, approved by our local ethics committee (approval no. 1208741), was conducted at the Royal (Dick) School of Veterinary Studies over 3 weeks. ResultsA total of 40 dogs were enrolled in the study. The study population consisted of Labrador Retriever (n=9) Cocker Spaniel (n=8), mixed breed (n=4), Staffordshire Terrier (n=3), Lhasa Apso (n=2), Chihuahua (n=2), Bulldog (n=2), Chinese Crested (n=1), Dogue de Bordeaux (n=1), Burmese Mountain (n=1), Poodle (n=1), Border Terrier (n=1), Beagle (n=1), Yorkshire Terrier (n=1), Collie (n=1), Maltese (n=1), and Patterdale Terrier (n=1) breeds. There were 26 females (23 neutered and 3 intact) and 14 males (9 neutered and 5 intact). The median weight was 16.75 kg (range: 2–52.6) and the median age was 5.1 years (range: 0.2–13). When comparing the two devices, the CVs obtained with the MMVBP and the PMD were 4.09% and 3.86%, respectively. The overall mean SBP measured by the PMD and by the MMVBP were 153.3 ± 3.2 and 152.6 ± 3.7 mmHg, respectively; the means were not significantly different (p=0.77). The mean SBP values acquired with both devices differed from each other by < 10 and 20 mmHg in 70% and 93% of dogs, respectively. The correlation between sets of mean SBP values obtained from each device was very good ( r=0.8269; p < 0.0001) (Fig. 1). With the Bland–Altman analysis, MMVBP slightly underestimated SBP compared to PMD with a wide level of agreement (bias=−0.6 ± 13.1 mmHg, 95% LoA: −26.3 to 25.09) (Fig. 2). The TOD risk SBP scoring system classified 13 dogs with a score of 1, 13 with a score of 2, 8 with a score of 3, and 6 with a score of 4 when the MMVBP device was used; whereas when the PMD device was used, 12 dogs were classified with a score of 1, 14 with a score of 2, 8 with a score of 3, and 6 with a score of 4. Two of the dogs assigned with a score of 3 with the MMVBP device were scored with a score of < 3 (one with a score of 2 and the other with a score of 1) with the PMD device. The contrary also occurred: two of the dogs assigned with a score of 3 with the PMD device were scored with a score of < 3 (one with a score of 2 and the other with a score of 1) with the MMVBP device. No dogs were defined as hypotensive in the present study.
Fig. 1. Correlation between the MMVBP device and the PMD device for SBP assessment in 40 conscious dogs (r=0.8269; p < 0.0001). The solid line represents the coefficients of correlation; the dashed lines represent the 95% confidence intervals. MMVBP, Mano Médical Vet BP; PMD, Parks Medical Doppler; SBP, systemic blood pressure. DiscussionThe assessment of SBP in conscious veterinary patients is commonly achieved by noninvasive indirect methods. The PMD, for instance, is one of the most commonly used Doppler ultrasonography devices in veterinary practices across the world and is considered to be a reliable tool for the acquisition of SBP measurements in conscious dogs (Acierno et al., 2018). Its recent discontinuation from the market has prompted the need for replacement devices to be considered; however, data regarding the agreement between different Doppler devices is currently limited. The aims of the present study were to compare two Doppler devices, the PMD and the MMVBP, for the measurement of SBP in conscious dogs in the clinical setting. In this study, SBP analysis was performed in a total of 40 conscious dogs, and the mean SBP readings provided by the two Doppler devices were not statistically different. The correlation between devices was observed to be very good, reflecting that a change in SBP detected by the MMVBP likely reflects an identical change with the PMD device (Hinkle et al., 2003). Agreement between devices was assessed using a Bland–Altman plot, which indicated that the MMVBP tended to slightly underestimate SBP compared to the PMD. According to this plot, the mean difference (bias) for SBP between devices was not large, but the SD was, which consequently led to a wide LoA. The mean of the values acquired with both devices differed from each other by < 10 and 20 mmHg in 70% and 93% of dogs, respectively. As observed in Figure 2, in one dog, this difference was greater than 40 mmHg. Based on this study’s results, the authors believe the disparities observed between devices were likely attributable to intraindividual variability in SBP over time. As previously shown in both canine and feline patients, blood pressure can significantly change overtime with repeated measurements (Remillard et al., 1991; Sparkes et al., 1999). The sets of SBP measurements were obtained consecutively not simultaneously, therefore a degree of minute-to-minute variation in blood pressure is likely to have occurred. The average time for acquisition of a SBP reading usually ranges between 15 and 25 seconds; however, in some cases, this can take longer (Haberman et al., 2006). During this time, the handling of the patient could result in sudden elevations in SBP and consequently lead to an increased variability between measurements. Unfortunately, this situational hypertension (previously termed “white-coat” effect) can be difficult to completely eliminate even when an attempt is made to select amenable dogs (Marino et al., 2011; Acierno et al., 2018). The underestimation of SBP by the MMVBP may also have been influenced by the order in which the devices were used (the PMD device was always used first) as the dogs could have become acclimatized to the technique by the time the MMVBP was used. Retrospectively, it would have been better if the order the devices used was randomized.
Fig. 2. Bland–Altman plot for analyses of agreement between PMD and MMVBP for SBP measurement in 40 conscious dogs. The solid horizontal line represents the bias and the dotted lines represent 95% LoA (±1.96 SD from the mean between the two devices used). Note that the MMVBP device slightly underestimated SBP compared to the PMD device. LoA, limits of agreement; MMVBP, Mano Médical Vet BP; PMD, Parks Medical Doppler; SBP, systemic blood pressure. In this study, the CVs from the five consecutive SBP readings for the two devices were similar (4.09% for the MMVBP and 3.86% for the PMD), suggesting a clinically acceptable intra-observer repeatability of both devices. Similar CVs have been previously reported when Doppler ultrasonography devices, such as the PMD, were used (Hsiang et al., 2008; Chetboul et al., 2010; Wernick et al., 2012a). As suggested in the ACVIM consensus statement, categorization of SBP based on TOD risk can be useful when assessing the need for antihypertensive treatment (Acierno et al., 2018). In our study, four dogs (10% of the study population) were classified with a score of 3 (SBP between 160 and 179 mmHg) with one device but with a score below 3 with the other. This finding could have resulted in significantly different clinical outcomes, e.g., different SBP treatment or monitoring regimes, as per ACVIM consensus recommendations (for those without evidence of TOD). Such results suggest that this scoring system should be applied with caution and ideally be based on repeated sets of measurements obtained from the same dog over time (taking intraindividual variability in SBP into account). There were a number of limitations in this study. The small study population could have impacted on the level of agreement between the devices by decreasing the statistical power; a narrower level of agreement might have been seen if more dogs had been enrolled. While this is a potential limitation, lower sample numbers have been previously used in similar studies (Jepson et al., 2005; Chetboul et al., 2010; Wernick et al., 2012b). The inclusion of more dogs with an SBP ≥ 180 mmHg would have allowed for a more accurate evaluation of the agreement between devices under high SBP conditions (only eight dogs had an SBP ≥ 180 mmHg). There were also few dogs with a low SBP, but they were excluded because assessment could have" should be "There were also few dogs with low SBP because these were excluded if assessment could have The aim of this study was not to validate the MMVBP. Further research in which the performance of the MMVBP is compared to the gold standard direct method, ideally in conscious dogs, is needed to elucidate the device’s accuracy (Haberman et al., 2006; Seliškar et al., 2013). This would hopefully allow for refinement of the validation criteria for this device, as well as for the establishment of monitor-specific reference intervals (Jepson et al., 2005; Acierno et al., 2018). ConclusionIn conclusion, the results of the present study suggest that the MMVBP and the PMD can be used interchangeably for assessment of SBP in conscious dogs. The wide LoA observed between both devices were most likely associated with intraindividual variability in SBP over time. Clinicians should be aware of the possibility for clinically relevant discrepancies between sets of SBP measurements obtained at different times with either device. AcknowledgmentsThe authors would like to thank the owners of the dogs in this study for allowing their dogs’ inclusion, including Dr Hester Cheuk for handling all of the dogs so well. ReferencesAcierno, M.J., Brown, S., Coleman, A.E., Jepson, R.E., Papich, M., Stepien, R.L. and Syme, H.M. 2018. ACVIM consensus statement: guidelines for the identification, evaluation, and management of systemic hypertension in dogs and cats. J. Vet. Intern. Med. 32(6), 1803–1822. Bodey, A.R., Michell, A.R., Bovee, K.C., Buranakurl, C. and Garg, T. 1996. Comparison of direct and indirect (oscillometric) measurements of arterial blood pressure in conscious dogs. Res. Vet. Sci. 61(1), 17–21. Bosiack, A.P., Mann, F.A., Dodam, J.R., Wagner-Mann, C.C. and Branson, K.R. 2010. Comparison of ultrasonic Doppler flow monitor, oscillometric, and direct arterial blood pressure measurements in ill dogs. J. Vet. Emerg. Crit. Care 20(2), 207–215. Chetboul, V., Tissier, R., Gouni, V., de Almeida, V., Lefebvre, H.P., Concordet, D., Jamet, N., Sampedrano, C.C., Serres, F. and Pouchelon, J.L. 2010. Comparison of Doppler ultrasonography and high-definition oscillometry for blood pressure measurements in healthy awake dogs. Am. J. Vet. Res. 71, 766–772. Chetboul, V. 2015. Intra- and interoperator variability. In: Eds., de Madron, É., Chetboul, V., and Bussadori CBT-CE of the D and C. St. Louis, MI: Elsevier Masson, pp: 39–43. Finco, D.R. 2004. Association of systemic hypertension with renal injury in dogs with induced renal failure. J. Vet. Intern. Med. 18(3), 289–294. Haberman, C.E., Kang, C.W., Morgan, J.D. and Brown, S.A. 2006. Evaluation of oscillometric and Doppler ultrasonic methods of indirect blood pressure estimation in conscious dogs. Can. J. Vet. Res. 70(3), 211–217. Hinkle, D.E., Wiersma, W. and Jurs, S.G. 2003. Applied statistics for the behavioral sciences. J. Educ. Stat. 15(1), 84. Hsiang, T.Y., Lien, Y.H. and Huang, H.P. 2008. Indirect measurement of systemic blood pressure in conscious dogs in a clinical setting. J. Vet. Med. Sci. 70(5), 449–453. Jepson, R.E., Hartley, V., Mendl, M., Caney, S.M.E. and Gould, D.J. 2005. A comparison of CAT Doppler and oscillometric memoprint machines for non-invasive blood pressure measurement in conscious cats. J. Feline Med. Surg. 7(3), 147–152. Littman, M.P., Robertson, J.L. and Bovée, K.C. 1988. Spontaneous systemic hypertension in dogs: five cases (1981–1983). J. Am. Vet. Med. Assoc. 193(4), 486–494. Marino, C.L., Cober, R.E., Iazbik, M.C. and Couto, C.G. 2011. White-Coat effect on systemic blood pressure in retired racing greyhounds. J. Vet. Intern. Med. 25(4), 861–865. Remillard, R.L., Ross, J.N. and Eddy, J.B. 1991. Variance of indirect blood pressure measurements and prevalence of hypertension in clinically normal dogs. Am. J. Vet. Res. 52(4), 561–565. Sansom, J. and Bodey, A. 1997. Ocular signs in four dogs with hypertension. Vet. Rec. 140(23), 593–598. Seliškar, A., Zrimšek, P., Sredenšek, J. and Petrič, A.D. 2013. Comparison of high definition oscillometric and Doppler ultrasound devices with invasive blood pressure in anaesthetized dogs. Vet. Anaesth. Analg. 40(1),21–27. Sparkes, A.H., Caney, S.M.A., Kind, M.C.A. and Gruffydd-Jones, T.J. 1999. Interand intraindividual variation in Doppler ultrasonic indirect blood pressure measurements in healthy cats. J. Vet. Intern. Med. 13(4), 314–318. Stepien, R.L. and Rapoport, G.S. 1999. Clinical comparison of three methods to measure blood pressure in nonsedated dogs. J. Am. Vet. Med. Assoc. 215(11), 1623–1628. Vachon, C., Belanger, M.C. and Burns, P.M. 2014. Research in veterinary science evaluation of oscillometric and Doppler ultrasonic devices for blood pressure measurements in anesthetized and conscious dogs. Res. Vet. Sci. 97(1), 111–117. Wagner, A.E. and Brodbelt, D.C. 1997. Arterial blood pressure monitoring in anesthetized animals. J. Am. Vet. Med. Assoc. 210(9), 1279–1285. Wernick, M.B., Höpfner, R.M., Francey, T. and Howard, J. 2012a. Comparison of arterial blood pressure measurements and hypertension scores obtained by use of three indirect easurement devices in hospitalized dogs. J. Am. Vet. Med. Assoc. 240, 962–968. Wernick, M.B., Francey, T. and Howard, J. 2012b. Indirect measurement devices in hospitalized dogs. J. Am. Vet. Med. Assoc. 240(8):9–14. | ||
| How to Cite this Article |
| Pubmed Style Domingues M, Archontakis P, Bouvard J, Winter L, Gunn-moore D. Comparison between the Parks Medical Doppler and the Mano Médical Vet BP Doppler for recording indirect systemic blood pressure in conscious dogs. Open Vet. J.. 2022; 12(4): 562-566. doi:10.5455/OVJ.2022.v12.i4.19 Web Style Domingues M, Archontakis P, Bouvard J, Winter L, Gunn-moore D. Comparison between the Parks Medical Doppler and the Mano Médical Vet BP Doppler for recording indirect systemic blood pressure in conscious dogs. https://www.openveterinaryjournal.com/?mno=103729 [Access: December 03, 2025]. doi:10.5455/OVJ.2022.v12.i4.19 AMA (American Medical Association) Style Domingues M, Archontakis P, Bouvard J, Winter L, Gunn-moore D. Comparison between the Parks Medical Doppler and the Mano Médical Vet BP Doppler for recording indirect systemic blood pressure in conscious dogs. Open Vet. J.. 2022; 12(4): 562-566. doi:10.5455/OVJ.2022.v12.i4.19 Vancouver/ICMJE Style Domingues M, Archontakis P, Bouvard J, Winter L, Gunn-moore D. Comparison between the Parks Medical Doppler and the Mano Médical Vet BP Doppler for recording indirect systemic blood pressure in conscious dogs. Open Vet. J.. (2022), [cited December 03, 2025]; 12(4): 562-566. doi:10.5455/OVJ.2022.v12.i4.19 Harvard Style Domingues, M., Archontakis, . P., Bouvard, . J., Winter, . L. & Gunn-moore, . D. (2022) Comparison between the Parks Medical Doppler and the Mano Médical Vet BP Doppler for recording indirect systemic blood pressure in conscious dogs. Open Vet. J., 12 (4), 562-566. doi:10.5455/OVJ.2022.v12.i4.19 Turabian Style Domingues, Marina, Panagiotis Archontakis, Jonathan Bouvard, Luke Winter, and Danielle Gunn-moore. 2022. Comparison between the Parks Medical Doppler and the Mano Médical Vet BP Doppler for recording indirect systemic blood pressure in conscious dogs. Open Veterinary Journal, 12 (4), 562-566. doi:10.5455/OVJ.2022.v12.i4.19 Chicago Style Domingues, Marina, Panagiotis Archontakis, Jonathan Bouvard, Luke Winter, and Danielle Gunn-moore. "Comparison between the Parks Medical Doppler and the Mano Médical Vet BP Doppler for recording indirect systemic blood pressure in conscious dogs." Open Veterinary Journal 12 (2022), 562-566. doi:10.5455/OVJ.2022.v12.i4.19 MLA (The Modern Language Association) Style Domingues, Marina, Panagiotis Archontakis, Jonathan Bouvard, Luke Winter, and Danielle Gunn-moore. "Comparison between the Parks Medical Doppler and the Mano Médical Vet BP Doppler for recording indirect systemic blood pressure in conscious dogs." Open Veterinary Journal 12.4 (2022), 562-566. Print. doi:10.5455/OVJ.2022.v12.i4.19 APA (American Psychological Association) Style Domingues, M., Archontakis, . P., Bouvard, . J., Winter, . L. & Gunn-moore, . D. (2022) Comparison between the Parks Medical Doppler and the Mano Médical Vet BP Doppler for recording indirect systemic blood pressure in conscious dogs. Open Veterinary Journal, 12 (4), 562-566. doi:10.5455/OVJ.2022.v12.i4.19 |